It’s been about 2.5 months with my 670G pump. I’ve never had such an intense love/hate relationship with a medical device before. When asked if I’d recommend the pump or how I feel about, my honest answer is that I have very mixed feelings about it. And I think the most important takeaway is to have realistic expectations if you decide to get this pump. It is far far from perfect, but it has incredible potential. However, there are many and frequent frustrations, and for me, the pump was not only affecting my sleep (which obviously has implications for all areas of your life), it was also affecting my mood.
One thing I’ve learned over the past 17 years living with a chronic disease is that you have to make it fit into your lifestyle, not the other way around. That doesn’t mean you don’t make changes to the way you live, but it also means that to get through each and every day, you find ways to fit diabetes into the life you want to live. I have a few diabetes mantras, and one of them is “Diabetes does not define you.” My health and safety is always my first priority, but within the confines of this pump, I’ve found some tricks to get me through each day so that the pump is not negatively affecting my mood and sleep.
I’ll stop right here and say that what I’m about to tell you is not the way that the pump was designed and intended to work, so if you choose to try any of the tricks below, you do so at your own risk. I’m not recommending these for everyone, obviously you know what is realistic or not for your own life and circumstances. But this blog is for sharing my personal experiences so that’s what I’m doing.
My 670G Tips and Tricks
1.Be very careful about when you calibrate. Medtronic seems to have a lot of advice about this, don’t calibrate when you’re rising or dropping, don’t calibrate when there’s active insulin, calibrate about 4 times a day. I’ve also found that since I’m a stomach/side sleeper, I try not to calibrate when I first wake up even if it’s asking for one. I give it 30 minutes to an hour for the sensor to even back out. When I get into the cycle that says “Wait to enter BG” sometimes it helps to wait more than the 15 minutes, up to an hour even before entering the next BG.
2. Learn your sensor’s patterns. The sensor is supposed to last 7 days, however this has rarely been my experience. Here’s what my sensor timeline typically looks like:
- Day 1: sensor is getting used to my body and usually isn’t very accurate for the first 24 hours.
- Day 2-4: Sensor typically works pretty well, calibrations last close to 12 hours.
- Day 5: Things start going downhill, either it will say change sensor or will need much more frequent calibrations.
- Day 6-7: Hah
3. Adapt your manual and auto mode use to your sensor’s patterns. I’ve found that when the sensor is in auto mode, it requires many more calibrations, and that it is much quicker to not accept a calibration and eventually tell you to change a sensor than if it’s in manual mode. This makes sense. Since it’s giving insulin in auto mode, it wants to make sure it’s as safe and accurate as possible. However, if you want your sensor to get the full 7 days (or as close as you can), you can sometimes stretch the use by staying in manual mode for the last couple days. Here’s how it works:
- Day 1: I keep it in manual mode for most of the day until the sensor is reading pretty close to my finger readings.
- Day 2-4: Auto mode
- Day 5: This is often where I get to the point that it tells me to change sensors. So now instead of cursing and getting mad, I disconnect the sensor from my body and charge it while turning off the sensor on my pump. Then I reconnect the sensor and “trick” the pump, telling it that it’s a new sensor. I then go through the warm-up period. For me, this works about half the time. If the sensor has gotten bent, then this trick won’t work, you’ll still end up changing it.
- Day 6-7: Manual mode
4. If you feel comfortable, alert silences can be a great thing. I always calibrate my sensor right before bed, hoping it will last the 12 hours. However, if you’re close to day 5 and beyond, the sensor will often ask for a calibration 6 hours later, which for me is around 4 or 5 am. I was waking so frequently that my body started automatically waking up at 5 am every morning, and I would have trouble falling back asleep. So now, I make a judgment call each night. If I feel pretty sure that my blood sugar isn’t fluctuating too much, I sometimes choose to silence all alerts for the night. This way it won’t wake me up if it needs a calibration. I did find that it does still vibrate for low blood sugars. The pros: an undisturbed night of sleep. The cons: if it does need a calibration during the night, you won’t have any readings and if you’re in auto mode, it probably will eventually kick you out. So ultimately this comes down to what you’re personally comfortable with. I don’t silence the alerts every night, more so for the nights I just really want an undisturbed night. And I’ve always been able to feel my lows during the night so I don’t rely as heavily on the pump alerts. Then if I wake up at 4 or 5 in the morning, I’ll often calibrate anyway. But at least then it’s my body waking me up, and not my pump.
Everyone’s needs and experiences are different. My “tricks” might not work for you or fit your lifestyle or may not be how you want to be using the pump. But maybe they do help. Either way, I’m all about sharing and learning from one another.



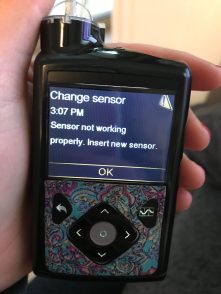 Yesterday, after wearing the sensor for 3 days, I got a message that the sensor was updating and then a message that said, “Change sensor. Sensor not working properly insert new sensor.” In that moment I was furious. I screamed obscenities in my head at my sensor and texted my boyfriend the picture of that screen with 10 emojis of the middle finger and angry faces.
Yesterday, after wearing the sensor for 3 days, I got a message that the sensor was updating and then a message that said, “Change sensor. Sensor not working properly insert new sensor.” In that moment I was furious. I screamed obscenities in my head at my sensor and texted my boyfriend the picture of that screen with 10 emojis of the middle finger and angry faces. It has literally only been about 2 hours since I turned this feature on and I’m sitting looking at one of the straightest, steadiest, in-range blood sugar graphs and I can’t help but get emotional. I have tears falling down my cheek as I type this. I don’t know that I can communicate everything that I’m feeling right now. For some of you, maybe you can relate, and for others, I hope I can come close.
It has literally only been about 2 hours since I turned this feature on and I’m sitting looking at one of the straightest, steadiest, in-range blood sugar graphs and I can’t help but get emotional. I have tears falling down my cheek as I type this. I don’t know that I can communicate everything that I’m feeling right now. For some of you, maybe you can relate, and for others, I hope I can come close. Just the idea that this pump is literally asking me to give up a lot of control, trust the sensor, and let the pump do some of the work is simultaneously terrifying and liberating. It takes away just a little of the burden of living with diabetes, but even that little bit counts for so much! And I am so grateful and excited that a pump with a feature like this finally, finally exists. The fact that I potentially won’t have as many roller coaster highs and lows is such an incredible thought that is almost too good to be true.
Just the idea that this pump is literally asking me to give up a lot of control, trust the sensor, and let the pump do some of the work is simultaneously terrifying and liberating. It takes away just a little of the burden of living with diabetes, but even that little bit counts for so much! And I am so grateful and excited that a pump with a feature like this finally, finally exists. The fact that I potentially won’t have as many roller coaster highs and lows is such an incredible thought that is almost too good to be true. We planted 2 kale plants, one beet plant and some chives. I’ll admit, it was pretty amazing to see the transformation of the plants in just a few weeks time. My garden consultant would examine the plants and tell me when to water and how much, helped spray the plants with organic pesticides and just generally kept an eye on how things were going.
We planted 2 kale plants, one beet plant and some chives. I’ll admit, it was pretty amazing to see the transformation of the plants in just a few weeks time. My garden consultant would examine the plants and tell me when to water and how much, helped spray the plants with organic pesticides and just generally kept an eye on how things were going.

 it’s the same one that I had practically written-off as a failure. I’m sorry I doubted you, kale. You survived the worm invasion and came out even bigger and stronger than before.
it’s the same one that I had practically written-off as a failure. I’m sorry I doubted you, kale. You survived the worm invasion and came out even bigger and stronger than before.