Wow, hi, it’s been a minute. Over two years, actually. I think we can all agree it’s been a very challenging past couple of years, and a lot has changed since my last post. The biggest change- I have a 7-month-old son! When I first started this blog, I thought that if/when I got pregnant, I would share the entire journey. Being pregnant with type 1 diabetes was always something that scared me, I honestly didn’t know if I could achieve and maintain the type of blood sugar control that I needed in order to have a safe pregnancy for me and the baby. Spoiler alert: I did it! But it was hard, and this pregnancy took a lot of physical, mental, and emotional energy. I just did not have enough energy left to document the journey. So instead, here I am 7 months later sharing my experience in hopes that it might help someone who may be having similar fears and doubts.
Becoming a parent is transformative on so many different levels. You learn so much about caring for a tiny, helpless human, but you also learn a lot about yourself in the process. Even before my son was born, he taught me that I can overcome challenges. I can face what scares me. What an invaluable lesson and one that I will teach and instill in him as well. And those 39 weeks were certainly challenging. The level of discipline and vigilance to keep my blood sugars between 65-140 all day, every day, was exhausting. But I’m not perfect and I had to learn not to get caught up in the “what ifs” and the worries when my blood sugar occasionally spiked above those levels. Having a high-risk pregnancy added an extra layer of anxiety that I knew I was taking on, but you don’t fully understand just what it entails until you’re in it (that very first doctor apt where they list off all the potential complications and risks was INTENSE). Not to mention the time/energy commitment going to over 40 doctor appointments over the course of my pregnancy between the ultrasounds, office visits, weekly phone calls with the diabetes educator, and twice a week non-stress tests at the end of the pregnancy. It was a lot, but worth every second!
So how did I do it? Before I tell you what worked for me, I do have to say that it’s important to follow the recommendations from your healthcare provider. My experience is not meant to be medical advice, just sharing what was helpful for me.
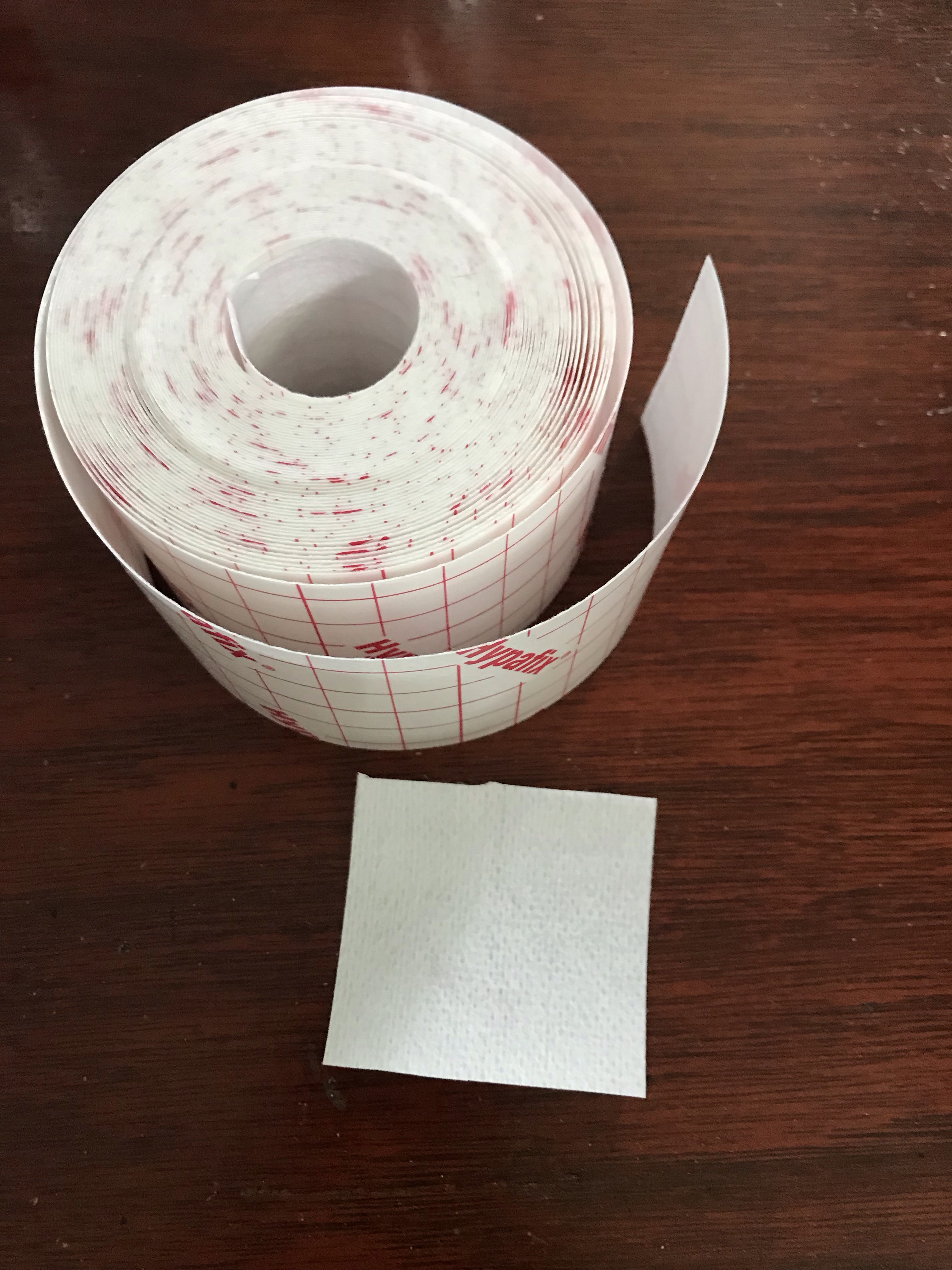
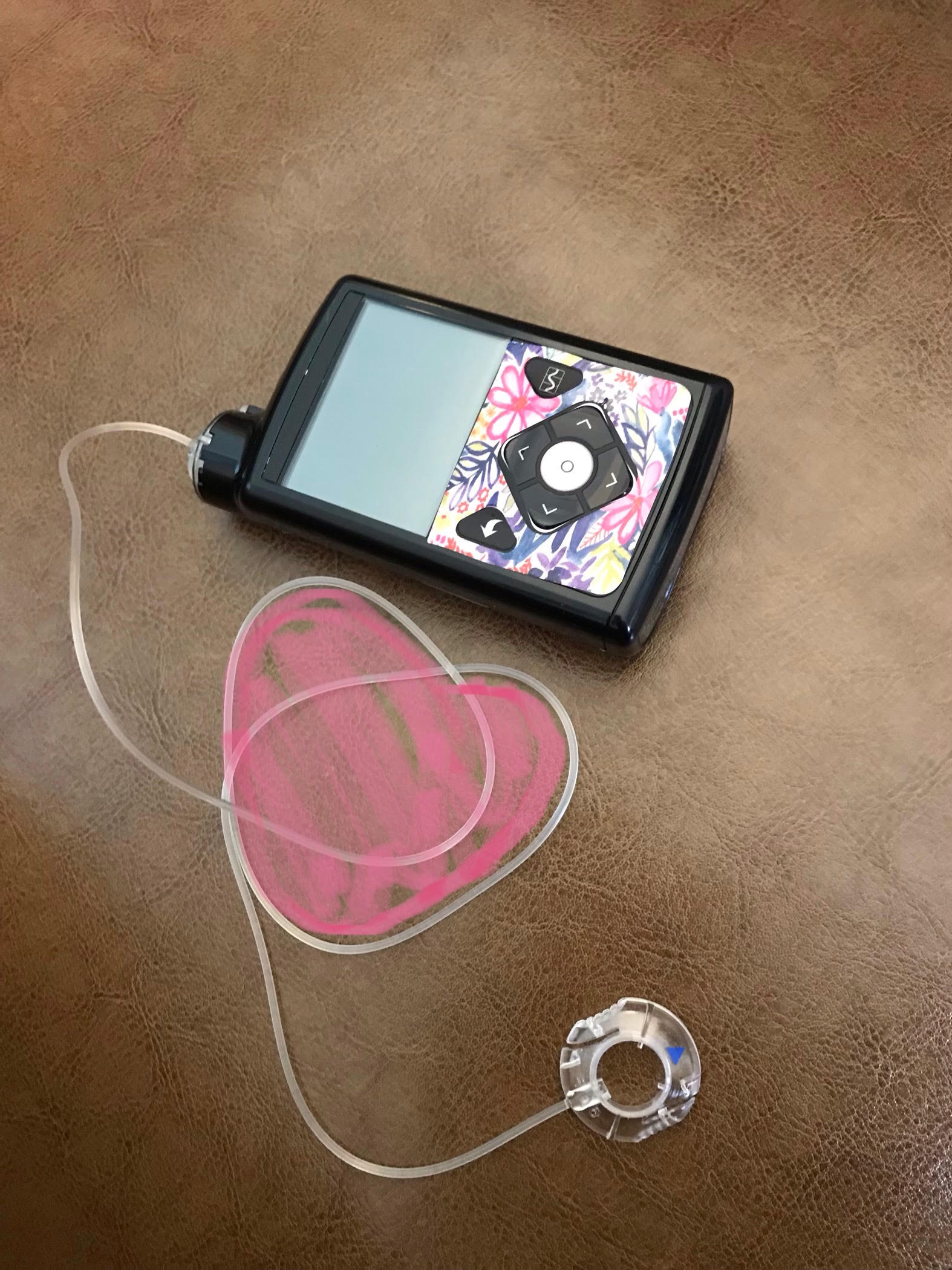
1. I had an amazing team of doctors and diabetes educators. Every week I had an appointment with a nutritionist/diabetes educator. She would look at my Dexcom glucose numbers from the past week and my pump settings, and make adjustments. While we didn’t really restrict anything I was eating, she had helpful suggestions for the timing and types of snacks to eat. When the insulin resistance kicked in, we were ready. These continuous and often minor tweaks made a big difference in making sure that my insulin needs were aligned with changes in my body. I really believe her constant reassurance and encouragement were integral to my success. With so many doubts and fears circling, hearing someone say “You’re doing really great” goes a long way.
2. I got better about pre-bolusing. I’ve always been bad about this, but I stepped it up when it mattered. And when I remembered to pre-bolus 15-30 min before my meal, it definitely helped my blood sugar spike less.
3. I set tighter ranges for high and low alerts so that I would be alerted early when blood sugars were rising or starting to get too high, especially at night. Yes, my alarms would wake me up at night a lot, but I was already waking constantly to go to the bathroom. This helped make sure that my blood sugars were never sitting too high for an extended amount of time overnight. And every time I would wake up in the night, I would check my blood sugar and make any needed corrections. I have an Apple watch where I can see my Dexcom blood sugars, so it was very convenient to look at my watch and see how I was doing.
4. I was extra vigilant when it came to my blood sugars and probably overly aggressive. Anytime I saw my arrows starting to trend upwards, I would set temp basals or give a correction to anticipate a spike. I set a LOT of temp basals, I found them to be very helpful. I erred on the side of giving too much insulin and risking going low rather than seeing too many high blood sugars. This may not be the best approach for everyone, but it’s what worked for me.
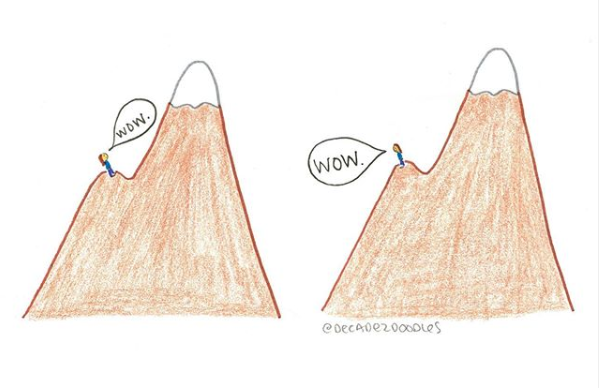
5. I did the best I could and learned to accept that some things are just out of my control. I learned not to freak out about a handful of high blood sugars now and then. My doctors repeatedly told me how well I was doing and that the time in range was more important than a few isolated incidents. Because as diabetics know, you can do the same exact thing as yesterday, eat the same meal, give the same insulin, and your blood sugar can behave completely differently. I think this was mentally the hardest part. Even before your baby is born, there’s this fierce need to protect them from harm and the “mom (parent) guilt” can make you doubt yourself. It’s hard to overcome these types of thoughts, but the fact that you’re even having them means you’re already a great parent.
So what’s my advice for any pregnant type 1 diabetics or anyone hoping to become pregnant? I would say make sure you have a team of doctors who you trust and are in constant communication with so that you can work together to fine-tune your insulin throughout your pregnancy. It’s okay to be scared, all emotions are important and valid, but don’t let your fear hold you back. And then do the best you can each day (knowing that no one is perfect) and take things one day at a time. You can do this!! When you hold your little one, it will make all the challenges worth it.


 better, but not much. Sensors rarely last the 7 days, almost every time I inserted a new sensor, it would just show my blood sugar dropping even when it wasnt, eventually rejecting the calbriations and telling me to change the sensor. Every day would require multiple calibrations with misleading arrows, causing even greater roller coaster blood sugars. I admit that automode was useful, but I would only end up being in automode less than half the time. The other 50% of the time was incredibly frustrating.
better, but not much. Sensors rarely last the 7 days, almost every time I inserted a new sensor, it would just show my blood sugar dropping even when it wasnt, eventually rejecting the calbriations and telling me to change the sensor. Every day would require multiple calibrations with misleading arrows, causing even greater roller coaster blood sugars. I admit that automode was useful, but I would only end up being in automode less than half the time. The other 50% of the time was incredibly frustrating. couldn’t believe how close they were. And then I lost it, I just started crying. It was like this weight I had been carrying around for 2 years was suddenly lifted. Like I had been holding my breath and I could finally breathe. I couldn’t believe the relief I felt, I hadn’t even known it was negatively affecting me so much.
couldn’t believe how close they were. And then I lost it, I just started crying. It was like this weight I had been carrying around for 2 years was suddenly lifted. Like I had been holding my breath and I could finally breathe. I couldn’t believe the relief I felt, I hadn’t even known it was negatively affecting me so much.