Two months ago, I had an appointment with a new endocrinologist. Back with my old endo, I made the decision to try for much tighter blood sugar control. Part of that decision involved getting off auto mode, switching to the Dexcom sensor, and having more frequent visits and check-ins with my health care team.
After years of my a1c hovering around 7, I wanted it to finally make it into the 6’s. And it happened! Not only was it in the 6’s, it was in the lower half of the 6’s. I couldn’t believe it!
The downside of this being a brand new doctor is that she didn’t know me, or my struggle to bring it down over the many years. She didn’t recognize what a huge accomplishment this was for me. I had imagined this exact moment for so long, I remember thinking, would I cry of happiness? Would my doctor share my excitement? Not that she wasn’t pleased, but the conversation quickly continued. And it continued to a much heavier topic. I wanted to know more about pregnancy and type 1 diabetes because at some point, when we’re ready, I want to start a family. And I wanted to know what that journey would look like for me so I could be prepared- physically, mentally, and emotionally. As one might expect, it will be a lot of work. Constant monitoring, adjusting, and tracking to keep blood sugars in a safe range for 9 months. My feelings of triumph and accomplishment were quickly overtaken by feelings of anxiety and fear. I had accomplished my first goal, getting into the 6’s, but suddenly there was so much more ahead of me when I decide to go down this path. It was daunting.
This whole experience reminded me of an illustration by one of my favorite Instagram artists/doodlers, decade2doodles.
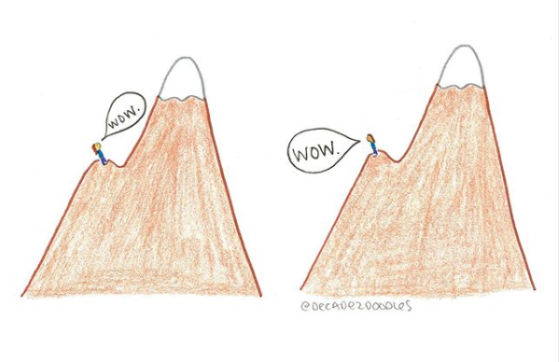
Here I was at the top of that first hilltop and instead of taking a moment to realize how far I had come, to celebrate that first victory, I was already looking ahead at how much more I needed to climb.
“When you’re scared about what’s next, find confidence in what came before.” This is what the artist had written below this post. The first time I saw this illustration, I don’t know if I even read what was below it, I related enough to the image itself. But the truth is, I look at this journey of pregnancy with type 1 diabetes and I am terrified! What if I can’t keep such strict blood sugar control? The risks with pregnancy are scary enough without adding in type 1 diabetes.
Now with another appointment next week, I’m afraid that I have taken a few steps backwards and I know my a1c will reflect that. “…find confidence in what came before.” I’m working on that confidence part. I got my a1c down to the 6’s, if I did that once, I know I’m capable of doing it again, of continuing to make improvements, and maintaining that level. And when I’m ready to climb that second part of the mountain and start a family, I know I’ll have the support of great doctors, family, and friends helping me along the way.

 All day I alternated between being livid and just feeling sad. I felt let down by the numbers I rely on every minute of the day to be healthy. By the end of the day, I made the decision to switch back to my old, reliable sensor. Enough is enough. My health shouldn’t be made worse by the devices that are meant to improve it.
All day I alternated between being livid and just feeling sad. I felt let down by the numbers I rely on every minute of the day to be healthy. By the end of the day, I made the decision to switch back to my old, reliable sensor. Enough is enough. My health shouldn’t be made worse by the devices that are meant to improve it.